Inaugural Health Equity Summit - Parts 1 & 2
Developing a Model of Healthcare for People with I/DD in the Washington, DC Region
Corresponding author: David A. Ervin, BSc, MA, FAAIDD
HELEN, The Journal of Human Exceptionality, presents – in a two-part series – proceedings of the Inaugural Health Equity Summit: Developing a Model of Healthcare for People with Intellectual and/or Developmental Disabilities in the Washington, DC Metropolitan Area. As readers will see, a group of clinicians, health policy experts, people with IDD, family members, home and community-based service providers, researchers and advocates from the region and from across the country convened a novel approach to community planning around a single focus, health equity for people with IDD.
Part 1 offers a statement of the issue and how the Summit was convened, its purposes and objectives, and reviews a number of models of care, including particular focus on healthcare financing as one of the significant barriers to healthcare access by people with IDD.
In Part 2, authors review how a healthcare delivery system that focuses on but is not necessarily exclusively and only for people with IDD is best organized, key components of a system of care, critical policy, research and health profession education initiatives in support of developing and sustaining such a system of care, and a review of the model contemplated for the Washington, DC metro area.
Questions can be directed to the corresponding author.
Introduction
There is no longer much debate on health disparities experienced by people with intellectual and/or developmental disabilities (IDD). In September, the National Institutes on Minority Health and Health Disparities (NIMHD) designated people with disabilities, including IDD, as a population with health disparities for research supported by the National Institutes of Health (NIH). This proclamation follows several others since the turn of the 21st Century that have highlighted disparities in access to healthcare, health status, social determinants of health, and health outcomes experienced by people with IDD.
These important pronouncements bring attention and critical resources to health advocacy work to address, fully and finally, stubborn and persistent barriers to accessible healthcare that is culturally relevant and responsive to the lived experiences of people with IDD and their health outcomes. Knowing there are these disparities is not enough. Creating solutions to resolve them is an urgent and long overdue priority.
“stubborn and persistent barriers to accessible healthcare that is culturally relevant and responsive to the lived experiences of people with IDD and their health outcomes.”
Abstract
Adults with IDD experience poorer health status and higher mortality and morbidity when compared to people without IDD. There are many well-researched reasons for this, including longstanding and persistent obstacles to accessible, culturally competent healthcare. Notable obstacles are the paucity of physicians and other health professionals who have received curriculum-based education or formal training in developmental medicine. There are persistent challenges in the use of public (e.g., Medicaid and Medicare) and private health insurance and reimbursement systems that do not adequately account for the needs of adults with disabilities whose healthcare encounters require more time, who benefit from access to specialty equipment that enhances healthcare experiences (e.g., high/low exam tables, wheelchair scales), and who experience different and substantial risk factors for poorer health status. In addition, longstanding attitudes among healthcare practitioners that originate in a time in history when disability and disease were held essentially as synonymous continue to inform barriers to appropriate care that delivers optimal health outcomes. In May 2022, Makom, a community provider of home and community-based services to people with IDD, convened a novel planning retreat. The purpose of the Health Equity Summit was to conceptualize a healthcare delivery system that focuses on and is tailored to the healthcare needs of adults with IDD in the Washington, D.C. metropolitan area. Attending the Summit were clinicians with an established commitment to and expertise in treating patients with IDD, health profession educators and students, health policy advocates and makers and government officials, people with IDD, family members of people with IDD, and community providers. Held over two days, the Summit resulted in a concept model for both the delivery of accessible, culturally relevant and integrated healthcare, as well as a substantial commitment to and structure in support of educating health profession students, including medical school students.
Keywords: developmental disabilities, developmental medicine, health disparities, healthcare, intellectual disability, proceedings
Introduction
Adults with intellectual and/or developmental disabilities (IDD) experience poorer health and significant barriers to accessible, quality healthcare (Anderson et al., 2013; Ervin et al., 2014; Krahn, et al., 2006). This has been especially highlighted during the COVID-19 pandemic, which has had a substantially more severe impact on people with IDD when compared to their peers without IDD (Landes et al., 2021; Turk et al., 2020). Among many barriers to accessible, culturally relevant and responsive healthcare are lack of formal training and education in health profession and medical school curricula, resulting in physicians and other health professionals being ill-informed, unprepared and uncomfortable in providing care (Bacherini, Havercamp and Balboni, 2021; Holder et al., 2009; Iezzoni et al., 2021; Wilkinson et al., 2012); financial barriers to accessible care, including challenges specific to Medicaid coverages and rates of reimbursement (Shady et al., 2022), and lack of resources dedicated to architectural and physical accessibility; and, lack of accessible wellness and health promotion resources and interventions, from routine preventative screenings (e.g., mammograms for women with IDD) to health behavior resources that are otherwise widely available to the general population (e.g., smoking/tobacco cessation, sexual health education) (Scott and Havercamp, 2016; Spassiani et al., 2019; Steenbergen et al., 2017).
Photo Credit: Rick Guidotti for Positive Exposure
Emerging trends in our understanding of healthcare for people with IDD suggest that the population will be best served by not only an improvement in the knowledge of healthcare professionals who do not specialize in IDD, but with the development and proliferation of healthcare providers and systems that do specialize in IDD. Functionally, people with IDD exist on a spectrum. The neurodevelopmental causes of IDD tend to result in intellectual disability, sensory differences, communication difficulties, neuromotor dysfunction, seizure disorders, and/or behavioral/psychiatric and mental health needs. These six domains are frequently overlapping, and it is often the case that the more severely these domains are impacted, the more severely other domains will be impacted as well. This essentially results in a multiplicative impact on medical complexity (M. Holder, personal communication, December 15, 2022). This complexity of the population contributes to significant healthcare utilization and requires a more specialized approach in delivering wellness, health promotion and healthcare services to people with IDD.
“A small number of model healthcare systems have been pioneering accessible healthcare that is designed for adults with IDD.”
A small number of model healthcare systems have been pioneering accessible healthcare that is designed for adults with IDD. For example Premier Healthcare, founded in 1997, includes healthcare clinics in four boroughs of New York City. This health system accepts all types of patients, with a specialty in treating adults with IDD. In the last 20 years, additional models have emerged that have been designed around the healthcare needs and experiences of people with IDD. Examples include the Achievable Health Center in California, the Lee Specialty Clinic in Kentucky, the Developmental Disabilities Health Center in Colorado, and the Developmental Disabilities Centers of the Atlantic Health System in New Jersey. While not an exhaustive list of systems of care, the development of these and other models in the last two decades is significant and impressive. However, while access to culturally competent healthcare for adults with IDD in communities in which new and existing models exist is substantial, there are scant such models in many communities. For adults with IDD in those rural, inner city, and other communities, access barriers have not improved, and health disparities persist.
Photo Credit: Lee Specialty Clinic Louisville, KY
One such community is in the Washington, D.C. region, including the suburban areas surrounding the city in both Maryland and Virginia, which combine to comprise what is colloquially referred to as the DMV (District of Columbia, and counties in both Maryland and Virginia that are contiguous or in close proximity to the District of Columbia). Beginning in approximately 2005, Georgetown University provided approximately 4000 consultations annually to as many as 800 people with IDD in the District of Columbia’s (D.C.) disability community, through a contract with D.C.’s Developmental Disabilities Administration (DCDDA) in issues that included complex medical care, training for nurses and direct support professionals (DSP), hospital transitions, home visits, sexual health, end-of-life consultations, and quality assurance studies. This contract ended in August 2019, from which time there is no formal healthcare system that focuses particularly on D.C. adult residents with IDD. Across the DMV, in fact, there are no dedicated systems of healthcare that, like the model healthcare systems shown above, specialize or tailor health services to adults with IDD. It is worth noting that among barriers to the creation of such a system are the complexities associated with three different jurisdictions comprising the region, each with its unique governing authorities and regulations for both healthcare and long term services and supports (LTSS)/home and community based services (HCBS) systems.
In May 2022, Makom, a community provider of HCBS supporting people with IDD in Maryland and Virginia, convened the inaugural Health Equity Summit: Developing a Model of Healthcare for People with Intellectual and/or Developmental Disabilities in the Washington, DC Metropolitan Region (Summit). This novel approach to community healthcare planning brought clinicians, health policy experts, self- and institutional advocates, family members, government officials, health profession educators, researchers and others, all with content and related expertise, to a two-day planning retreat (list of attendees is provided in Appendix A). The stated purpose of the Summit was twofold:
To conceptualize a healthcare delivery system for the DMV that specializes in culturally accessible and competent healthcare for people with IDD; and,
To develop a work plan to bring the concept model to fruition.
The agenda (Appendix B) was comprised of the following broad items:
Review current state, statement of need
Identify existing health resources—i.e., hospital systems, medical and health profession education institutions, county and state resources, and more
Review current models of excellence for potential application of similar frameworks to the local region
Conceptualize the chosen model for the region
Outline next steps, design implementation framework
Summit
There has been and continues to be debate as to the best approach to take in addressing health and healthcare access disparities experienced by people with IDD. One side of the debate holds that the current system of healthcare must be made fully inclusive. That is, healthcare outlets (e.g., clinics, physician offices) must allow for patients with IDD and patients without IDD. The alternative argument focuses on tailored specialty healthcare outlets that cater exclusively to patients with IDD. Harris (2006) noted that “to provide the best care and the best support, knowledge about neurogenic syndromes, management of biomedical and behavior features, psychosocial interventions, and the natural history of the [IDD] are critical. Background knowledge and sensitivity to the needs and life challenges of the affected person is especially important” (p. 11).
More recently, Lauer and colleagues (2021) studied hospital and emergency department (ED) utilization by people with IDD. They noted that substantial use of hospital and ED services are for conditions/presenting issues better addressed in ambulatory care settings and underscored that for primary care practitioners who can deliver competent care for people with IDD. As noted, there are very few medical schools and health profession education curricula that deliver critical training on the care and needs of people with IDD, a natural consequence of which is vast numbers of physicians and other health professionals being ill-informed, unprepared and uncomfortable in providing care (Holder et al., 2009; Iezzoni et al., 2021; Wilkinson et al., 2012).
In the DMV, only Georgetown University School of Medicine, Community Health Division offers medical professional training that specifically focuses on adults with IDD through a community-based learning model. Additionally, as the region covers three jurisdictions, and multiple counties, coalescing the diverse available health provider entities into a unified regional system of care for the general population is highly improbable. It is perhaps more probable that an interstate compact might lead to a coordinated specialty referral and delivery system that focuses more narrowly on healthcare for adults with IDD. This would involve a significant commitment on the part of the three government entities, as well as Congress, which oversees Washington, D.C.
“It is perhaps more probable that an interstate compact might lead to a coordinated specialty referral and delivery system that focuses more narrowly on healthcare for adults with IDD. This would involve a significant commitment on the part of the three government entities, as well as Congress, which oversees Washington, D.C.”
Against this reality, the expectation that the current healthcare system be made comprehensively more accessible and deliver better health outcomes to adults with IDD with coordinated care in the DMV is unlikely to be met anytime soon. The alternative approach is to create a specialty healthcare outlet that focuses on people with IDD and is built as a healthcare collaborative comprised of a coalition of health service providers, health education institutions, and also engages and is integrated with the LTSS and other systems of care, with support from governments within the DMV, is seen as ideal. Such a system, in addition to providing accessible, culturally relevant and responsive, comprehensive healthcare, will also allow for specific training and/or specifically trained physicians and other health professionals to deliver ambulatory care to people with IDD. This model would thus not only be an ambulatory care option for people with IDD, but also a novel teaching/training center for both health profession students and established health professionals seeking to learn developmental medicine.
Summit attendees discussed advantages and challenges in both approaches, ultimately forming consensus around the need to create a specialty care delivery system to both provide culturally competent and accessible, integrated multidisciplinary healthcare to people with IDD and to use such a healthcare delivery system as a training and professional development resource to elevate the competence and confidence of health professionals across the broader healthcare system in the Washington, D.C. metropolitan region.
Models of Care
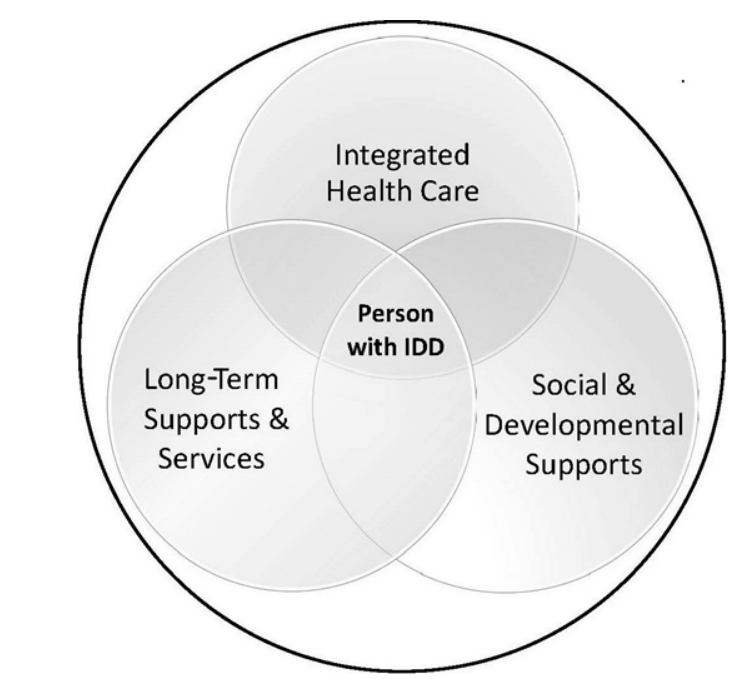
Over the last 20 years in the United States, there has been progress in addressing barriers to accessible and culturally relevant healthcare. New and emerging models of healthcare—several detailed above—have been developed and preliminary data suggest improving health outcomes. For example, Wilson, et al. (2020) examined health outcomes of patients of the Developmental Disabilities Health Center (DDHC), and found statistically significant improvements in rates of hypertension, hyperlipidemia, and certain mental health concerns, as well as clinically significant reductions in weight. A critical element to the DDHC model was the presence of a Cross-Systems Care Integration manager whose function was to integrate systems of care (Figure 1), thus bringing far more comprehensive resources to the health of the patient than just traditional primary and specialty healthcare practitioners in a traditional care coordination role.
The Lee Specialty Clinic in Kentucky is a comprehensive ambulatory care clinic featuring medical (primary and specialty), mental and behavioral health, dental care and a host of specialty disciplines including allied health, in one place. YAI Premier Healthcare in New York City offers similarly robust integrated multidisciplinary care in a health home model. Bobbette and colleagues’ (2021) research suggests a health home model is a preferred approach to delivering optimal care to patients with IDD, allowing for interprofessional collaboration for practitioners and ease and convenience for patients.
There are also models of care that are not, on their own, direct healthcare providing models. For example, the Philadelphia Coordinated Health Care (PCHC), the Southeast Region Health Care Quality Unit (HCQU) and one of eight HCQUs in Pennsylvania, works with adults with IDD and their families to access existing healthcare resources in the Philadelphia metropolitan area. This model includes nurses and behavioral health practitioners that are available on a consultative basis. However, PCHC’s focus is connecting adults with IDD in need of accessible healthcare to fully integrated, generally available healthcare resources.
Figure 1. DDHC Cross-Systems Care Integration
There are other models both established and emerging. For example, the Kramer Davis Clinic, a specialty integrated primary and specialty care clinic built on a value-based reimbursement framework, is scheduled for launch in Nashville, Tennessee in 2023. However, information exchange across and among models (e.g., a community of practice), and research on efficacy and effectiveness is limited (Sisirak and Marks, 2015). This has hampered more significant development of new models and innovation.
Finances
There are several reimbursement and payment schemes used by existing models of care. The Achievable Health Center and DDHC are both built on federally qualified health center (FQHC) platforms. The Health Resources and Services Administration (HRSA) defines an FQHC as a “community-based health care provider that receives funds from the HRSA Health Center Program to provide primary care services in underserved areas” or to underserved populations. Enhanced reimbursements are available to FQHCs, and while the vast majority of FQHC patients are publicly insured (i.e., Medicaid, Medicare) and uninsured, FQHCs also accept private insurance reimbursements.
Other models of care rely on traditional sources of both private insurance and public reimbursements. YAI Premier Healthcare accepts most major health insurance plans, Medicaid, Medicare and several dental insurance plans. The Westchester Institute for Human Development’s Medical Home, which serves 5500 patients with disabilities each year, a significant number of whom are patients with IDD, also accepts most insurances, and is built on a partnership with and as part of the University Center of Excellence in Developmental Disabilities (UCEDD) at New York Medical College. This model leverages medical and health profession students in clinical care, as well as offering access to patients at a host of teaching hospitals. Funding for the Lee Specialty Clinic is provided by the Centers for Medicare and Medicaid Services (CMS) and the Kentucky Cabinet of Health and Family Services, Department for Behavioral Health, Developmental and Intellectual Disabilities on a cost-based reimbursement structure.
It is estimated that 60% of the 7.4 million Americans with IDD are enrolled in Medicaid. Only 17% receive Medicaid- or state-financed long-term services and supports (Larson, et al., 2021). In the DMV, the number of people with IDD enrolled in Medicaid is approximately 43,000, with fewer than 12,800 receiving Medicaid- or state-funded long-term support. This leaves many people with IDD in the region covered by private insurance (children and adult children to age 26) by a parent, in few cases where the person with an IDD is covered by private insurance through an employer, and some who will be uninsured altogether.
Summit attendees reviewed these and other reimbursement systems. Generally, existing reimbursement systems are an acknowledged barrier to access to and quality of healthcare for people with IDD (Ervin and Merrick, 2014; Fujiura, Li & Magana, 2018; US Department of Health and Human Services, 2002). The potential need for a longer encounter to accommodate the communication needs of a patient with IDD, for example, is not aligned with reimbursement systems that base payment on standard 15-minute encounters. The FQHC platform potentially allows for enhanced rates, is cost-based, and is likely a preferred option in developing healthcare systems for people with IDD. Another potentially useful model is in Medicaid managed care (MMC), which has the potential of integrating care across both the traditional healthcare system and LTSS/HCBS. Maryland, Washington, DC, and Virginia all offer Medicaid managed care options, although none currently include people with IDD receiving Medicaid-financed Home and Community Based Services (HCBS).
This concludes part one. Part two discusses the organization, findings, and recommendations from the summit and will appear in the December issue of HELEN.
Corresponding author: David A. Ervin, BSc, MA, FAAIDD. Chief Executive Officer, Makom. 1500 East Jefferson Street, Rockville, MD, 20852, USA; +1.240.283.6001. E-mail address: dervin@makomlife.org
1) David A. Ervin, Makom, Rockville, MD; 2) Sara Ailey, Department of Community, Systems and Mental Health Nursing, Rush University, Chicago, IL; 3) James C. Bridgers, Department of Health and Human Services, Montgomery County, MD; 4) Marisa C. Brown Georgetown University Center for Excellence in Developmental Disabilities; 5) Kim Bullock, Community Health Division, Department of Family Medicine, Georgetown University School of Medicine, Washington, D.C.; 6) Sydnee Chavis, Department of Oral Surgery, University of Maryland School of Dentistry, College Park, MD; 7) Melissa DiSipio, Philadelphia Coordinated Health Care (PCHC), Philadelphia, PA; 8) Steven M. Eidelman, Department of Human Development and Family Sciences, University of Delaware, Newark, DE; National Leadership Consortium on Developmental Disabilities; 9) Craig Escudé, IntellectAbility, Clearwater, FL; 10) Donyale Hobson-Garcia, Trudy R. Jacobson, Matthew P. Janicki, University of Illinois at Chicago, Chicago, IL; National Task Group on Intellectual Disabilities and Dementia Practices; 11) Nicole LeBlanc, Rachel London, Maryland Developmental Disabilities Council, Baltimore, MD; 12) Benjamin Margolis, Access: Supports for Living, Orange County, NY; American Academy of Developmental Medicine and Dentistry, Warwick, NY; 13) Nesreen Shahrour, Maureen van Stone, Maryland Center for Developmental Disabilities at Kennedy Krieger Institute; Project HEAL (Health, Education, Advocacy, and Law); Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 14) Sheryl White-Scott, Metro Developmental Disabilities Service Office, Bronx, NY; AHRC New York City, New York, NY; Department of Medicine, New York Medical College, Valhalla, NY; 15) Kate Williams, Mark S. Wolff, University of Pennsylvania School of Dental Medicine, Philadelphia, PA
Inaugural Health Equity Summit - Part 2
Dec 1
Developing a Model of Healthcare for People with I/DD in the Washington, DC Region
Corresponding author: David A. Ervin, BSc, MA, FAAIDD
HELEN, The Journal of Human Exceptionality, presents – in a two-part series – proceedings of the Inaugural Health Equity Summit: Developing a Model of Healthcare for People with Intellectual and/or Developmental Disabilities in the Washington, DC Metropolitan Area. As readers will see, a group of clinicians, health policy experts, people with IDD, family members, home and community-based service providers, researchers and advocates from the region and from across the country convened a novel approach to community planning around a single focus, health equity for people with IDD.
Part 1 offers a statement of the issue and how the Summit was convened, its purposes and objectives, and reviews a number of models of care, including particular focus on healthcare financing as one of the significant barriers to healthcare access by people with IDD.
In Part 2, authors review how a healthcare delivery system that focuses on but is not necessarily exclusively and only for people with IDD is best organized, key components of a system of care, critical policy, research and health profession education initiatives in support of developing and sustaining such a system of care, and a review of the model contemplated for the Washington, DC metro area.
The consolidated, full article is available here. Questions can be directed to the corresponding author.
Organization
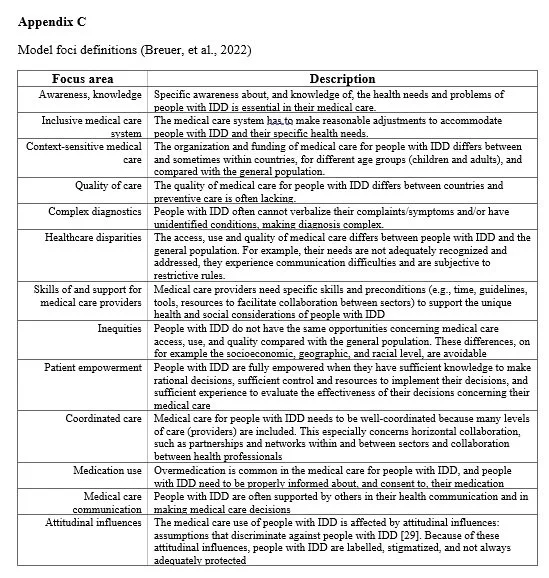
Breuer and colleagues’ (2022) analyses of major elements of medical care for people with IDD provides a framework for developing a care delivery system. Of note from this framework are emphases on patients with IDD taking active roles in their healthcare, integration of care and interprofessional collaboration, and training and professional development resources for healthcare providers. These foci represent longstanding barriers to quality healthcare and health outcomes for people with IDD, as well as aspirations to optimal healthcare and resulting outcomes, are represented in Figure 2 (definitions for each of the 13 categories are in Appendix C).
Figure 2. Healthcare System Elements (Breuer, et al., 2022)
Using this framework and based on core principles around which Summit attendees formed consensus, it was noted that a healthcare delivery system for the Washington, DC metropolitan area should include:
Primary and specialty healthcare, dental, behavioral and mental health, allied and ancillary care.
Integration with the long-term services and supports/Home and Community Based Services system of care (e.g., through a model similar to DDHC’s Cross System of Care Integration).
Social care services that focus on addressing and mitigating adverse social determinants of health and maintaining healthy living situations, health promotion and wellness.
Significant and formal training and professional development for healthcare practitioners already practicing throughout the region; and, partnership with local medical and/or health profession schools to develop clinical rotation opportunities, community based learning, residency opportunity and post-residency fellowships.
Consultative model, in addition to direct service, to both people with IDD and their families (similar to PPHC) and physicians and other healthcare professionals across the community.
Formal health promotion and wellness services to enhance health literacy, provide health-related resources (e.g., tobacco cessation materials, sexual education, etcetera), brain health initiatives (e.g., weight reduction and maintenance, exercise and physical activity, and nutrition counseling) that are cognitively accessible.
University-connected research on service delivery, health outcomes, health related quality of life, and other measures of impact and effectiveness
System Components
Summit attendees reviewed potential partners to the development of a healthcare delivery system that are likely to expand capacity and increase impact. For example, several existing models reviewed, notably the Westchester Institute for Human Development Medical Home, include critical partnerships with hospital systems. Another essential component of any healthcare delivery system for people with IDD is the need to develop formal professional development and health profession practitioner training opportunities in partnerships with medical, dental and health profession universities. Additional components assessed as important are shown in Table 1, as well as reasons for them.
Additional considerations include the need for training resources for health professionals who are out of their formal education programs and already practicing in their discipline, the need for a universal (shared) electronic health record (EHR) system that can integrate with data collection and documentation systems, including diagnoses codes to identify people with IDD in data analyses, that are common in the Home and Community Based Services system, and the need to create robust training opportunities for specialty care providers (e.g., Association of Psychology Postdoctoral and Internship Centers, or APPIC).
Table 1. Priority Components and Rationale
Policy and Research
There are significant barriers to health equity that can be addressed through policy advocacy, research and dissemination of information. (Financing and reimbursements are addressed above.) Among recommendations from the 2015 National Goals in Health and Wellness Research, Policy, and Practice (Sisirak and Marks, 2015) was the creation of an Information Exchange to “provide (a) open access to research outputs (e.g., innovative health and wellness programs, best practices, new findings, etc.); (b) policy and practice monographs and reports; and (c) promising technology that informs best practices for facilitating health care delivery, health advocacy, inclusion, and self-determination for people with IDD, their families, and supports” (p. 244). Another recommendation was to create and sustain a community of practice to identify existing and emerging models of care and compare the efficacy and effectiveness of those models, particularly around health outcomes, costs of care, health-related quality of life, and practitioner experience to inform policy. Further, the system must address best practice models with relation to teaching and inculcating healthy lifestyle and self-maintenance health practices and provide the supports to implement and maintain such programs to improve general wellness (Santos et al., 2022). Additional policy priorities to both inform the development of a model in the Washington, DC metropolitan region, as well as to create a public and health equity policy agenda that such a model and its stakeholders would pursue, include the following:
Implementation of value-based reimbursement (VBR) system that incentivizes improved health outcomes and health-related quality of life.
Medically Underserved Population (MUP) designation by HRSA for people with IDD—at the federal level and/or at the individual state level.
Public insurance/universal coverage of alternative medicine(s).
Required minimum, curriculum-based training in health profession curricula that explicitly addresses the healthcare and health needs and experiences of people with IDD and includes hands-on clinical experiences.
Creation of clinical competence metrics and formal standards of care focused on people with IDD. (See American Board of Developmental Medicine for Diplomate requirements at https://abdm.org/.)
Improving and expanding representation of people with IDD in health status surveillance data to inform policy (Havercamp, et al., 2019).
Integration of LTSS/HCBS and healthcare systems via collective cooperative agreements among the regions IDD agencies, health providers, and appropriate local government jurisdictions.
Summit attendees identified strategic collaborations in support of policy priorities, including the appropriate Developmental Disabilities Council (for any of Maryland, Washington, DC, and/or Virginia), state and/or local medical, dental, nursing and related societies, The Arc of the United States and/or state chapters, and major community providers of LTSS/HCBS to adults with IDD and their families.
A commitment to evaluating measurable, demonstrable impacts and effectiveness of the healthcare delivery system contemplated by Summit attendees was identified as a priority. Consistent with another of the 2015 National Goals in Health and Wellness Research, Policy and Practice (Sisirak and Marks, 2015) “to identify, document and compare the efficacy and effectiveness of existing models of community-based health care services…specifically looking at improved health outcomes including patient centered outcomes and cost of care” (p. 243), research priorities to align with the development of a healthcare delivery system for people with IDD in the Washington, DC region include at least:
Longitudinal impact on biomarkers (see, for example, Wilson, et al., 2020), health-related quality of life (e.g., Pett, et al., 2021), patient and provider satisfaction, and utilization of healthcare resources.
Comparing models of care across common patient outcome measures—this will involve sharing de-identified datasets with other systems of care, with a priority of publishing those comparisons in the scientific literature.
Dissemination of research will be through peer-reviewed/juried scientific journals, presentations at regional, national, and international conferences, and providing training opportunities (seminars, webinars and other formats) for clinicians across the Washington, DC region and virtually to clinicians anywhere. Potential partners in creating a research agenda include, for example, Kennedy Krieger Institute, Maryland’s University Center of Excellence in Developmental Disabilities (UCEDD) and Leadership Education in Neurodevelopmental and Related Disabilities (LEND), University of Maryland School of Dentistry, University of Pennsylvania School of Dental Medicine, and at a national level but in the Washington, DC area, the National Institutes of Health, National Institutes of Mental Health, National Institute on Aging, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Education and Professional Development
The absence of IDD content in health profession curricula is well established. The result is health professionals who are unequipped and uncomfortable in treating people with IDD, which in turn negatively impacts their health status and outcomes. The National Council on Disability has prioritized the formal inclusion of disability clinical-care competency in health profession curricula (National Council on Disability, 2022). While there is progress in adding IDD content to health profession and medical school curricula (e.g., University of Colorado School of Medicine added 10 hours of disability content to its curriculum, a part of which focuses on cognitive disabilities, in 2021), it is slow. More common are a host of promising didactic, experiential, and community-based learning modules (Golub-Victor et al., 2022; Troller et al., 2018).
The National Inclusive Curriculum in Health Education (NICHE; previously known as National Curriculum Initiative in Developmental Medicine), a project of the American Academy of Developmental Medicine and Dentistry (AADMD), seeks to provide training to medical students in the field of developmental medicine & inspire a medical career focused on individuals with IDD across the lifespan (American Academy of Developmental Medicine and Dentistry, n.d.). For physicians who are beyond the formal medical school-based education, the American Board of Developmental Medicine has begun certifying physicians who specialize in the care of people with IDD in order to increase expertise and specialty recognition.
Summit attendees unanimously urged the inclusion of formal training and professional development for health profession students in the many schools and universities in the region. The Westchester Institute for Human Development model includes a residency elective rotation in Developmental Medicine, for example. In Washington, DC, Georgetown University School of Medicine, Community Health Division, has dedicated educational resources to teaching IDD competence across disciplines, and is a willing collaborator in the creation of accessible and competent health services in the metropolitan region.
In addition, attendees spoke to the need to offer continuing medical/health education resources to health practitioners across disciplines already established in the community. To this purpose, collaboration with state, county or local medical societies is a priority. Partnerships with organizations such as IntellectAbility, which offer specialty training on IDD healthcare to clinicians on a virtual platform to develop clinical competence, are considered natural extensions of the education and professional development imperative for a healthcare delivery system for people with IDD in the Washington, DC metropolitan area. Other organizations with which to collaborate are the AADMD and the Developmental Disabilities Nurses Association (DDNA), which offer robust training, professional development and accreditation/certification resources for practicing clinicians; and, the University of Pennsylvania School of Dental Medicine offers continuing education specifically designed for professionals interested in treating people with IDD, as well as hands-on immersion training for dental teams.
Access to resources to improve health literacy among people with IDD, as well as direct support professionals (DSP) with whom they work, must improve. Given the need for integration of care across both (at least) the home and community-based services and healthcare systems, Summit attendees agreed on the need to develop and share these resources among caregivers, including DSPs but also including family caregivers and other natural supports (Geukes, Broder and Latteck, 2019; Overwijk et al., 2022;). Health promotion materials (e.g., tobacco cessation, human sexuality) that are developed to be culturally and cognitively accessible and disseminated widely to people with IDD and their caregivers is considered an essential element. A cooperative agreement among the DMV’s providers of LTSS/HCBS to adults with IDD would include concurrence to share training and education resources and offer common use and practices training for the personnel of all providers.
Summary
The agenda (Appendix B) for the Inaugural Health Equity Summit focused on first conceptualizing a healthcare model built with and for people with IDD in the Washington, DC Metropolitan Region, and second on developing a workplan to move the concept into practice. The conceptual model is a community-based healthcare collaborative of key partners and essential components as described above, and is established and designed to provide multidisciplinary, integrated healthcare to patients with IDD. The convening of the relevant DMV authorities with jurisdiction over IDD services and supports (e.g., the Maryland Developmental Disabilities Administration), public health authorities, and other, similar entities is an essential initial step to scope practicalities of interstate/inter-jurisdictional agreements. Engaging appropriate Developmental Disabilities Councils, area community providers of supports to adults with IDD, and advocacy organizations to review practicalities of and avenues to producing a regional agreement on cooperative health services is another early, key step. This macro-level focus is paramount to gaining consensus and agreement on how best to meet the healthcare and wellness needs and expectations of adults with IDD in the region.
Additional components include designing a model for training and ongoing professional development resources to any health profession practitioner in the Washington, DC region to improve confidence and increase competence among all practitioners and provide training opportunities for health profession students; dedicated health advocacy in support of policy initiatives at a local, state and federal level; a research hub and community of practice, to inform and learn from established and emerging best practices; and, a dedicated resource to improve health literacy among people with IDD , their DSPs, and other caregivers. A workplan, in support of these imperatives, is developed to establish the model. Several but not all priorities in the workplan are to continue to engage and rely on self-advocates on model design elements, to clearly identify partners to the model and the manner by which (for example, a memorandum of understanding or similar) they are engaged, and to work closely with both public and private insurances on creating the reimbursement models.
The COVID-19 pandemic revealed vulnerabilities in physical and mental health among people with IDD (Gleason, et al., 2021). There are several reasons for this, including higher rates of chronic morbidities and poorer access to culturally competent healthcare provided by trained and supported healthcare practitioners. The COVID-19 crisis and its impact on people with IDD is a call to action. In 2001, a Special Olympics-commissioned report (Horowitz, et al., 2001) outlined 13 recommendations to “remediate [healthcare] problems” experienced by people with IDD (p. 157-159. This was followed by 16th US Surgeon General David Satcher’s watershed report, Closing the Gap: A National Blueprint to Improve the Health of Persons with Mental Retardation (US Public Health Service, 2001) which outlined six goals and action steps to address health disparities long common among people with IDD. More than 20 years later, progress has been slow. In the Washington, DC metropolitan area, there remains a range of persistent barriers to healthcare that is accessible and specifically competent treating patients with IDD. The Inaugural Health Equity Summit: Developing a Model of Healthcare for People with Intellectual and/or Developmental Disabilities in the Washington, DC Metropolitan Region and its attendees have developed a model of healthcare for this community of people and a workplan to achieve it.
Acknowledgements
The Inaugural Health Equity Summit: Developing a Model of Healthcare for People with Intellectual and/or Developmental Disabilities in the Washington, DC Metropolitan Region was supported by an anonymous donor to the Makom Innovation Fund. This Proceedings manuscript was co-authored by Summit attendees, whose contributions to the Summit and commitment to the work that has followed is extraordinary. The authors thank Dr. Matthew Holder for his contributions to writing and editing the manuscript.
Authors report no conflicts of interest.
Corresponding author: David A. Ervin, BSc, MA, FAAIDD. Chief Executive Officer, Makom. 1500 East Jefferson Street, Rockville, MD, 20852, USA; +1.240.283.6001. E-mail address: dervin@makomlife.org
1) David A. Ervin, Makom, Rockville, MD; 2) Sara Ailey, Department of Community, Systems and Mental Health Nursing, Rush University, Chicago, IL; 3) James C. Bridgers, Department of Health and Human Services, Montgomery County, MD; 4) Marisa C. Brown Georgetown University Center for Excellence in Developmental Disabilities; 5) Kim Bullock, Community Health Division, Department of Family Medicine, Georgetown University School of Medicine, Washington, D.C.; 6) Sydnee Chavis, Department of Oral Surgery, University of Maryland School of Dentistry, College Park, MD; 7) Melissa DiSipio, Philadelphia Coordinated Health Care (PCHC), Philadelphia, PA; 8) Steven M. Eidelman, Department of Human Development and Family Sciences, University of Delaware, Newark, DE; National Leadership Consortium on Developmental Disabilities; 9) Craig Escudé, IntellectAbility, Clearwater, FL; 10) Donyale Hobson-Garcia, Trudy R. Jacobson, Matthew P. Janicki, University of Illinois at Chicago, Chicago, IL; National Task Group on Intellectual Disabilities and Dementia Practices; 11) Nicole LeBlanc, Rachel London, Maryland Developmental Disabilities Council, Baltimore, MD; 12) Benjamin Margolis, Access: Supports for Living, Orange County, NY; American Academy of Developmental Medicine and Dentistry, Warwick, NY; 13) Nesreen Shahrour, Maureen van Stone, Maryland Center for Developmental Disabilities at Kennedy Krieger Institute; Project HEAL (Health, Education, Advocacy, and Law); Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 14) Sheryl White-Scott, Metro Developmental Disabilities Service Office, Bronx, NY; AHRC New York City, New York, NY; Department of Medicine, New York Medical College, Valhalla, NY; 15) Kate Williams, Mark S. Wolff, University of Pennsylvania School of Dental Medicine, Philadelphia, PA
References
American Academy of Developmental Medicine and Dentistry. (n.d.). Niche. Inclusive Curriculum. Retrieved March 6, 2023, from https://www.aadmd.org/niche
Anderson, L. L., Humphries, K., McDermott, S., Marks, B., Sisirak, J., & Larson, S. (2013). The state of the profession of health and wellness for adults with intellectual and developmental disabilities. Intellectual and Developmental Disabilities, 51(5), 385–398. https://doi.org/10.1352/1934-9556-51.5.385
Bacherini, A., Havercamp, S. M., & Balboni, G. (2021). Physicians' attitudes about individuals with intellectual disability and health care practices toward them: A systematic review. Psychiatria Danubina, 33(Suppl 11), 79–90
Bobbette, N., Lysaght, R., Ouellette-Kuntz, H., Tranmer, J., & Donnelly, C. (2021). Organizational attributes of interprofessional primary care for adults with intellectual and developmental disabilities in Ontario, Canada: A multiple case study. BMC Family Practice, 22(1), 157. https://doi.org/10.1186/s12875-021-01502-z
Breuer, M., Bakker-van Gijssel, E.J., Vlot-van Anrooij, K., Tobi, H., Leusink, G.L. & Naaldenberg, J. (2022). Exploring views on medical care for people with intellectual disabilities: an international concept mapping study. International Journal for Equity in Health, 21(1), 99. https://doi.org/10.1186/s12939-022-01700-w
Ervin, D.A., Hennen, B., Merrick, J., & Morad, M. (2014). Healthcare for persons with intellectual and developmental disability in the community. Frontiers in Public Health, 2, 83. https://doi.org/10.3389/fpubh.2014.00083
Ervin, D.A. & Merrick, J. (2014). Intellectual and developmental disability: Healthcare financing. Frontiers in Public Health, 2, 160. https://doi.org/10.3389/fpubh.2014.00160
Fujiura, G., Li, H. & Magaña, S. (2018); Health services use and costs for Americans with intellectual and developmental disabilities: A national analysis. Intellectual and Developmental Disabilities, 56(2): 101–118. doi: https://doi.org/10.1352/1934-9556-56.2.101
Geukes, C., Bröder, J. & Latteck, Ä.-D. (2019). Health literacy and people with intellectual disabilities: What we know, what we do not know, and what we need: A theoretical discourse. International Journal of Environmental Research and Public Health, 16. 463. 10.3390/ijerph16030463
Gleason, J., Ross, W., Fossi, A., Blonsky, H., Tobias, J. & Stephens, M. (2021, March 5). The devastating impact of covid-19 on individuals with intellectual disabilities in the United States. NEJM Catalyst Innovations in Care Delivery. Retrieved August 10, 2022, from https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0051
Golub-Victor, A.C., Peterson, B., Calderon, J., Lopes, A.D. & Fitzpatrick, D. (2022) Student confidence in providing healthcare to adults with intellectual disabilities: Implications for health profession curricula. Intellectual and Developmental Disabilities. Advance online publication, retrieved August 16, 2022 from http://aaidd.org/publications/journals/articles-accepted-for-publication
Harris, J.C. (2006). Intellectual disability: Understanding its development, causes, classification, evaluation and treatment. New York, NY: Oxford University Press.
Havercamp, S.M., Krahn, G.L., Larson, S.A., Fujiura, G., Goode, T.D., Kornblau, B.L. & National Health Surveillance for IDD Workgroup (2019). Identifying people with intellectual and developmental disabilities in national population surveys. Intellectual and Developmental Disabilities, 57(5), 376–389. https://doi.org/10.1352/1934-9556-57.5.376
Holder, M., Waldman, H. & Hood, H. (2009). Preparing Health Professionals to Provide Care to Individuals with Disabilities. International Journal of Oral Profession, 1, 66–71. https://doi.org/10.4248/ijos.09022
Horowitz, S., Kerker, B., Owens, P. & Zigler, E. (2001). The health status and needs of individuals with mental retardation. New Haven: Yale University School of Medicine. Special Olympics, Inc. Retrieved August 10, 2022 from https://dotorg.brightspotcdn.com/af/87/5834a3734eb7b21bf1660296df71/healthstatus-needs.pdf
Iezzoni, L.I., Rao, S.R., Ressalam, J., Bolcic-Jankovic, D., Agaronnik, N.D., Donelan, K., Lagu, T. & Campbell, E.G. (2021). Physicians' perceptions of people with disability and their health care. Health Affairs,40(2), 297-306. doi: 10.1377/hlthaff.2020.01452
Krahn, G., Hammond, L., & Turner, A. (2006). A cascade of disparities: Health and health care access for people with intellectual disabilities. Mental Retardation and Developmental Disabilities Research Reviews, 12(1), 70– 82. https://doi.org/10.1002/mrdd.20098
Krahn, G. L., & Fox, M. H. (2014). Health disparities of adults with intellectual disabilities: what do we know? What do we do? Journal of Applied Research in Intellectual Disabilities, 27(5), 431–446. https://doi.org/10.1111/jar.12067
Landes, S.D., Turk, M.A. & Ervin, D.A. (2021). COVID-19 case fatality disparities among people with intellectual and developmental disabilities: Evidence from 12 US jurisdictions. Disability and Health Journal, 14(4), 1-6. 10.1016/j.dhjo.2021.101116
Larson, S.A., van der Salm, B., Pettingell, S., Sowers, M., & Anderson, L.L. (2021). Long-term supports and services for persons with intellectual or developmental disabilities: Status and trends through 2018. Minneapolis: University of Minnesota, Research and Training Center on Community Living, Institute on Community Integration. Retrieved August 10, 2022 from https://ici-s.umn.edu/files/yFXkkmRteg/2018-risp-full-report?preferredLocale=en-US
Lauer, E., Lindgren, S., Momany, E., Cope, T., Royer, J., Cogan, L., McDermott, S. & Armour, B. (2021). Health service utilization patterns among Medicaid-insured adults with intellectual and developmental disabilities: Implications for access needs in outpatient community-based medical services. Journal for Ambulatory Care Management, 44(2), 138-147. doi: 10.1097/JAC.0000000000000373
National Council on Disability (2022, February). Health equity framework for people with disabilities. Washington, D.C. Retrieved August 16, 2022 from https://ncd.gov/sites/default/files/NCD_Health_Equity_Framework.pdf
Overwijk, A., Hilgenkamp, T.I.M., van der Schans, C.P., van der Putten, A.A.J. & Waninge, A. (2022). Development of a Dutch training/education program for a healthy lifestyle of people with intellectual disability. Intellectual and Developmental Disabilities, 60 (2), 163–177. Doi: https://doi.org/10.1352/1934-9556-60.2.163
Pett, M.A., Guo, J.W., Cardell, B., Johnson, E.P., Guerra, N. & Clark, L. (2021). Psychometric properties of a brief self-reported health-related quality of life measure (HRQoL-IDD) for persons with intellectual and developmental disabilities. Journal of Applied Research in Intellectual Disabilities, 34(3), 877–890. https://doi.org/10.1111/jar.12831
Santos, F. H., Zurek, J., & Janicki, M. P. (2022). Efficacy of healthy aging interventions for adults with intellectual and developmental disabilities: A systematic review. The Gerontologist, 62(4), e235–e252. https://doi.org/10.1093/geront/gnaa192
Scott, H.M. & Havercamp, S.M. (2016). Systematic review of health promotion programs focused on behavioral changes for people with intellectual disability. Intellectual and Developmental Disabilities, 54(1), 63–76. Doi: https://doi.org/10.1352/1934-9556-54.1.63
Shady, K., Phillips, S., & Newman, S. (2022). Barriers and facilitators to healthcare access in adults with intellectual and developmental disorders and communication difficulties: An integrative review. Review Journal of Autism and Developmental Disorders. doi: 10.1007/s40489-022-00324-8. Epub ahead of print.
Sisirak, J. & Marks, B. (2015). Health and wellness strand: Recommendations from National Goals Conference 2015. Inclusion, 3(4), 242–249. doi: https://doi.org/10.1352/2326-6988-3.4.242
Spassiani, N.A., Meisner, B.A., Abou Chacra, M.S., Heller, T., & Hammel, J. (2019). What is and isn't working: Factors involved in sustaining community-based health and participation initiatives for people ageing with intellectual and developmental disabilities. Journal of Applied Research in Intellectual Disabilities, 32(6), 1465–1477. https://doi.org/10.1111/jar.12640
Steenbergen, H.A., Van der Schans, C.P., Van Wijck, R., De Jong, J. & Waninge, A. (2017). Lifestyle approaches for people with intellectual disabilities: A systematic multiple case analysis. Journal of the American Medical Directors Association, 18(11). https://doi.org/10.1016/j.jamda.2017.06.009
Trollor, J.N., Eagleson, C., Turner, B., Tracy, J., Torr, J.J., Durvasula,S., Iacono, T., Cvejic, R.C. & Lennox, N. (2018). Intellectual disability content within tertiary medical curriculum: How is it taught and by whom? BMC Medical Education, (18), 182. https://doi.org/10.1186/s12909-018-1286-z
Turk, M.A., Landes, S.D., Formica, M.K., & Goss, K.D. (2020). Intellectual and developmental disability and COVID-19 case-fatality trends: Trinetx analysis. Disability and Health Journal, 13(3), 100942. https://doi.org/10.1016/j.dhjo.2020.100942
U.S. Public Health Service (2001). Closing the gap: A national blueprint for improving the health of individuals with mental retardation. Report of the Surgeon General’s Conference on Health Disparities and Mental Retardation. Washington, D.C. Retrieved August 15, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK44346/
Wilkinson, J., Dreyfus, D., Cerreto, M. & Bokhur, B. (2012). “Sometimes I feel overwhelmed”: educational needs of family physicians caring for people with intellectual disability. Intellectual and Developmental Disabilities, 50(3): 243–250. doi: https://doi.org/10.1352/1934-9556-50.3.243
Wilson, T., Geer, B., Guerra, N., Karber, B., & Ervin, D.A. (2020). Cross-systems care integration impact on adults with intellectual disability utilizing risk weight and comorbidity data: A comparative effectiveness study, 2014-2017. Intellectual and developmental disabilities, 58(5), 422–431. https://doi.org/10.1352/1934-9556-58.5.422
Appendix A
Inaugural Health Equity Summit: Developing a Model of Healthcare for People with Intellectual and/or Developmental Disabilities in the Washington, DC Metropolitan Region
Attendees
Appendix B
Appendix C
Model foci definitions (Breuer, et al., 2022)