FROM THE STACKS
EDITOR’S NOTE: There are literally thousands of journals published around the world that relate to the disability community. It is virtually impossible to capture even a fraction of them. HELEN receives "stacks" of journals and selectively earmarks what we feel are "must read" articles of interest for our readers. It's a HELEN perk.
NIH Brain Study for Teens ages 11-17 with Autism
Researchers are studying the brain’s response to language and sound. This investigational research study uses repetitive transcranial magnetic stimulation (rTMS), an investigational form of brain stimulation, to measure how different parts of the brain communicate in teens with autism spectrum disorder (ASD). Findings from this study may aid in the development of possible future treatments.
This outpatient study includes:
Brain imaging (MRI and MEG) Brain stimulation (rTMS) Neurobehavioral assessments. About 7 visits over 6 months
Volunteers must:
Be ages 11 to 17 years and able to agree to participate. Have ASD
Compensation may be provided up to $1,000.
- To learn more about this NIH study #20-M-0159, or other studies, please call us at 833-JOIN-NIH.
Interested in Participating in Research?
The NIH Clinical Center Research Hospital is looking for volunteers to help advance medical discoveries!
Neuropsychiatric Disorders Among Adult Emergency Department Patients With Intellectual and Developmental Disabilities
(Psychiatry Online - 9/04/2025)
Harold A Pollack 1 2, Brandon Tabman 3, Derek S Brown 4, Hefei Wen 5, Kristin L Berg 6, Lauren Peterson 1, Betsy Q Cliff 2, Beau M Ances 7, Kenton J Johnston 3
PMID: 40904051
Abstract
Objective: This study aimed to compare rates of psychiatric and neurologic diagnoses on emergency department (ED) visit records of adults with versus without intellectual and developmental disabilities (IDDs).
Methods: This cross-sectional study used the 2019 Nationwide Emergency Department Sample of U.S. hospital ED visit discharges. Validated codes were used to compare psychiatric and neurologic diagnoses of patients ages ≥18 with versus without diagnosed IDDs. Diagnosed psychiatric and neurologic conditions included depression, anxiety, schizophrenia or psychosis, suicidality, seizure, dementia, and sleep disorder.
Results: The analysis identified 558,408 and 112,593,527 (nationally weighted) ED visits by adults with and without IDDs, respectively. Compared with the general population, adults with IDDs were twice as likely to have a mental disorder as the principal visit diagnosis, with higher probabilities of principal visit suicidality (1.6 times higher), neurologic disorder (5.6 times higher), and seizure (8.1 times higher) diagnoses. Compared with the general population, adults with intellectual disability were nearly twice as likely to have a dementia diagnosis, and patients with Down's syndrome were six times likelier to have a dementia diagnosis. More than one in five ED visit records of patients ages 50-54 with Down's syndrome included a dementia diagnosis; the dementia diagnosis rate for such patients ages ≥70 was 2.7 times higher than that of the general population.
Conclusions: Adult ED patients with IDDs were more likely than those without IDDs to have co-occurring mental and neurologic disorders. Findings underscore the need to provide neuropsychiatric services across the lifespan to address the distinctive care needs of individuals with IDDs.
NADSP Policy Update: Recognizing the Role of Direct Support Professionals Act
Recently, a bipartisan group of congressional champions — Representatives Brian Fitzpatrick (R-PA) and Joe Morelle (D-NY), along with Senators Maggie Hassan (D-NH) and Susan Collins (R-ME) reintroduced the Recognizing the Role of Direct Support Professionals Act (H.R. 6137 / S. 3211). This legislation urges the Office of Management and Budget to finally establish a Standard Occupational Classification (SOC) specifically for Direct Support Professionals.
For many years, NADSP has made the creation of a DSP-specific SOC one of our highest national priorities. We have consistently argued that the federal government must formally recognize the unique, demanding, and highly skilled nature of direct support work. DSPs deserve a classification that reflects the real work they perform every day: supporting people with intellectual and developmental disabilities to live full, meaningful, self-directed lives in their communities.
A DSP-specific SOC is more than a bureaucratic update. It is a long overdue acknowledgment that the work you do is unique, professional, and complex.
A distinct SOC will finally allow states, intellectual disability programs, and policymakers to use accurate employment and wage data when setting reimbursement rates. This creates meaningful opportunities for wage advancement, greater career satisfaction, and a more stable IDD support system — all rooted in the truth that DSPs perform a unique job that cannot be reduced to generic caregiving.
NADSP has always maintained that without federal recognition of DSPs as a distinct occupation, the workforce crisis cannot be properly understood or solved. The reintroduction of this legislation represents a critical step toward building the data infrastructure needed to address chronic recruitment and retention challenges and to elevate the DSP profession to where it belongs.
Now is the time to ask your U.S. House Member and U.S. Senators to endorse the Recognizing the Role of Direct Support Professionals Act. This bipartisan bill offers a real chance to reshape the future of direct support. With bipartisan support, we hope that this is an issue that can unite both Republicans, Democrats, and the Administration.
Please take a moment to contact your Members of Congress and urge them to support the Recognizing the Role of Direct Support Professionals Act.Your advocacy will help ensure that direct support professionals finally receive the federal recognition, respect, and wage fairness they have earned. Together, we can strengthen this profession and improve the lives of the people with I/DD who depend on DSPs every day.
With appreciation and solidarity,
Joseph M. Macbeth, President & CEO, National Alliance for Direct Support Professionals
TAKE ACTION > Click the button below to contact your representatives. Now is the time to ask your U.S. House Member and U.S. Senators to endorse the Recognizing the Role of Direct Support Professionals Act.
An Updated Definition of Global Health
Kathryn H. Jacobsen, Caryl E. Waggett, Olusoji Adeyi, Walter Bruchhausen, Shahanaz Chowdhury, Patricia M. Davidson, Ximena Garzón-Villalba, Lawrence O. Gostin, Liz Grant, Philip J. Landrigan, Hao Li, Mario C. Raviglione, Nancy R. Reynolds, Nelson K. Sewankambo, Brittany Seymour & Keith W. Martin
Excerpt from Global Health Research and Policy volume 10, Article number: 56 (2025)
Abstract
The most cited definition of global health, published in The Lancet in 2009, defines global health as “an area for study, research, and practice that places a priority on improving health and achieving equity in health for all people worldwide”. In this article, we propose an updated definition that expresses the motivations of diverse global health actors and makes One Health and sustainability more visible: “Global health is a field of academic study, research, policy, and applied practice that advances the equitable protection and improvement of population and planetary health”. Our “5 Ps model” illustrates global health as a grid that places health for all at the center of two axes representing four domains: (1) People, (2) Planet, (3) Priorities, and (4) Policies and Practices. The people–planet axis spans from social, economic, political, and other systems that affect human health to complex worldwide challenges such as those related to globalization, migration, pandemics, and climate change. The priorities–policies/practices axis positions global health as an action-oriented field in which factors such as human rights, international law, the global burden of disease, and evidence of economic impact inform the financing, implementation, and evaluation of multisectoral partnerships and interventions. We propose using this updated definition and the 5 Ps framework to modernize discussions of the scope and purpose of global health.
Background
Global health was established as a distinct field in the late 1990s with the goal of replacing older, often colonial models of international health engagement with more equitable partnerships that respond to existential human threats while continuing to support improvements in population health in low- and middle-income countries. The new era of global health ushered in a broader array of funders, unprecedented resources for health, new public–private partnerships, and expanded roles for governments, businesses, and civil society organizations [1, 2]. Multilateralism and effective global governance, including greater transparency and accountability, were championed in this framing of global health, but some of the dominant actors downplayed critical questions about power imbalances, imperialism, aid dependency, and other tensions between the “Global North” and “Global South” [3].
Investment in global health surged in the early 2000s as the Millennium Development Goals (MDGs) established by the United Nations (UN) catalyzed international support for poverty reduction in 2000–2015 [4]. The documented successes of the MDG era prompted the UN General Assembly, in collaboration with UN Member States and hundreds of nongovernmental organizations, to adopt the more ambitious Sustainable Development Goals (SDGs) for 2016–2030 [5]. The SDGs were founded on the premise that narrowing the disparities between and within the world’s richest and poorest countries would yield lasting benefits for all collaborating parties while generating prosperity, preserving the planet, and fostering peace. As part of the SDG process, high-income countries made voluntary financial and technical commitments to accelerate progress on dozens of economic, health, environmental, and other targets in less-resourced countries.
The coronavirus pandemic that began in 2020 stalled progress on nearly all of the SDG targets and dampened enthusiasm for the concept of global goals even as it demonstrated the interdependence and shared vulnerabilities of all nations [6, 7]. The pandemic also revealed weaknesses in the International Health Regulations and in global governance structures and organizations, including the World Health Organization [8]. The strain on international relations during the pandemic foreshadowed the broader breakdown of global political norms in the post-pandemic years. By 2025, the United States and some other countries had begun withdrawing from participation in global governance and reframing equity, diversity, inclusion, and international cooperation as threats rather than strengths [9].
Global health has from its inception been motivated by a mix of economic considerations, humanitarian impulses, and biosecurity concerns [10]. All of these drivers of global health are currently being undermined by nationalistic and isolationistic movements that demand reduction of international aid and weaken the diplomatic cooperation required to mitigate shared threats like climate change, plastic pollution, armed conflict, and pandemics through treaties and other international instruments [11]. These rapid sociopolitical changes warrant an updated definition of global health that clarifies the scope and purpose of the field.
Current definition
The most commonly cited definition of global health, written by Jeffrey Koplan and the executive board of the Consortium of Universities for Global Health (CUGH) and published in The Lancet in 2009 as a viewpoint entitled “Towards a common definition of global health” [12], defines global health as “an area for study, research, and practice that places a priority on improving health and achieving equity in health for all people worldwide” and explains that “global health emphasizes transnational health issues, determinants, and solutions; involves many disciplines within and beyond the health sciences and promotes interdisciplinary collaboration; and is a synthesis of population-based prevention with individual-level clinical care”. Global health differs from public health in scope, governance, and complexity, with global health initiatives targeting health issues that have been prioritized at the international or global levels rather than at local or national scales and global health decision-making involving a more diverse set of multilateral and multisectoral actors than public health [12].
The definition by Koplan et al. has been adopted by numerous medical, public health, and other groups, in part because it presents an ambitious vision for what the field can ultimately accomplish. However, several updates would make this definition more relevant today. Two are especially important.
First, the Koplan definition emphasizes a vision for global health transformation more than the policy-based processes that are necessary for achieving this goal. We affirm that definition’s centering of the values and ideals of global health. A commitment to ensuring that all people and all communities have an equal opportunity to achieve their own best health status motivates many individuals and groups working in the multidisciplinary, interprofessional global health space [13]. Core principles like health equity, social justice, collaborative governance, and sustainability remain central to the field [14]. However, these tenets represent only part of the rationale for investment in global health. For example, governments, corporations, and philanthropists use global health to enhance their own security, strengthen their diplomatic efforts, exercise their power, expand commercial opportunities, and elevate their reputations. The Koplan definition highlights the strengths and aspirations of global health at its best but glosses over some of the strategic and political realities that also shape this multisectoral field. A more candid and comprehensive definition must express a broader set of motivations, mechanisms, and actors involved in global health prioritization, policymaking, financing, and implementation.
Second, the Koplan definition of global health, which predates the integrated cross-sectoral vision of the SDGs, focuses exclusively on human health. Since that definition was published, climate change, biodiversity loss, persistent pollution, and other forms of environmental degradation have come to be recognized as leading threats to the health and wellbeing of current and future generations [15]. Humans are interdependent with animals and ecosystems, as emphasized in the One Health approach, and all living things depend on a healthy Earth and healthy ecosystems for survival [16]. Because environmental sustainability is now recognized as essential to safeguarding human security, an updated definition of global health must make planetary health a visible priority [17, 18].
Proposed definition
Dozens of definitions of global health have been written in the years since the Koplan et al. paper was published, but that definition continues to be the most widely used one [19]. The paper presenting the definition has been cited thousands of times, and organizations in every world region feature the definition on their websites, in their institutional reports, and in their educational materials. Because this definition still holds significant weight in the field, we aim to modernize it while retaining its foundational structure. We therefore propose this update to the Koplan definition: “Global health is a field of academic study, research, policy, and applied practice that advances the equitable protection and improvement of population and planetary health”.
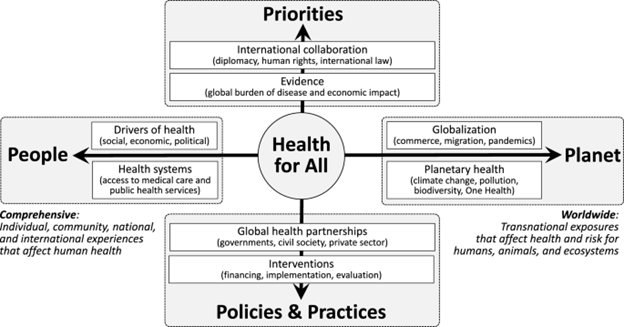
The key dimensions of a revised global health definition can be visualized using a grid that places health for all at the center of four domains: (1) people, (2) planet, (3) priorities, and (4) policies and practices. Figure 1 depicts this framework as a graph centered on health equity. The sample content provided for each domain is intended to be illustrative rather than exhaustive. Practitioners typically concentrate their work in one domain or quadrant, but the field as a whole comprises all parts of the graph [20].
Fig. 1
The 5 Ps model of global health
Health is protected through actions that advance human rights, attenuate risk factors, and prevent new public health threats in an equitable and just manner. The people–planet axis of the 5 Ps framework identifies the many shared problems that are amenable to preventive interventions, spanning from the full set of social, economic, political, and other factors that affect access to medical care and public health services through transnational threats like pandemics and climate change that require coordinated global responses and can affect human, animal, and ecosystem health. This axis expresses both the comprehensive and worldwide meanings of the word “global” in global health. The language of protection also evokes the importance of global health security, a responsibility that has motivated government participation in many global health partnerships and initiatives.
Health is improved through actions that ameliorate existing health concerns and generate progress toward achieving health equity [21]. The priorities–policies/practices axis summarizes the full scope of activities, from upstream governance through downstream implementation, that can increase healthy lifespans, resilience, and preparedness in communities and countries around the world. These actions span from international agreements and scientific evidence that shape global health agendas to the on-the-ground activities that contribute to solving prioritized health problems. This axis applies to both academic and applied global health work, positioning global health both as a discursive and an action-oriented field.
Implications for global health
Our proposed definition represents an incremental yet vital change for this interdisciplinary, interprofessional field. We acknowledge that this is not a transformative reimagining of global health in response to its critics, but we believe that it is necessary to clarify the current state of the field and build common ground across diverse worldviews so that stakeholders in global health can work more effectively together to shape a healthier future [22]. We have aimed to balance idealism and pragmatism in our definition, retaining health equity as the ultimate goal and framing global health as broad but not borderless. We affirm calls for continued reflection and dialogue about power dynamics and politics in global health to ensure that the field evolves in ways that are responsive to critical perspectives and changing global realities [23].
We write with a vision of strengthening, rather than abandoning, global health governance. Recognizing weaknesses in the current model of international collaboration is a critical first step toward improving the processes and structures that enable governments and their partner organizations to set effective policies, provide services, protect human rights, and build public trust. Since governments and governmental agencies may not always represent the best interests of their populations, especially in fragile states and nondemocratic settings, a model of global health that places the wellbeing of people at the center and welcomes contributions from a range of disciplines, professions, and sectors will be better equipped to meet complex health challenges now and create more effective, inclusive, transparent, accountable, and resilient systems for the future.
As leaders within CUGH and other global health organizations, we advocate for a transition from the original definition by Koplan et al. to this amended definition. We believe that this updated definition and the 5 Ps framework—people, planet, priorities, policies and practices—can enrich conversations about the field’s scope, relevance, and value and modernize how the field of global health is conceptualized and applied in teaching, research, and policy contexts.